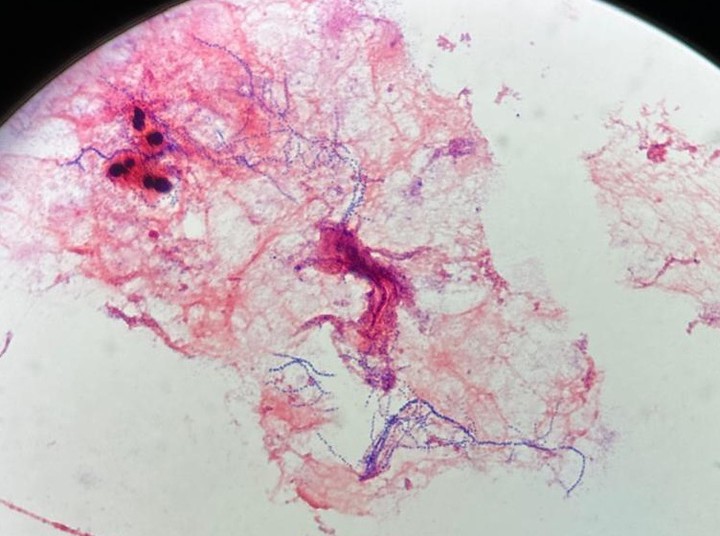
Nocardia farcinica is a gram-positive, partially-acid fast, filamentous, rod-shaped bacteria that is found in organic soil matter1. Infections of the brain parenchyma by Nocardia are rare and can pose a challenge to treat.
A 58-year-old male presented to the hospital with multiple abscesses. Six weeks prior, the patient had a chicken coop with exposed wire fall across his anterior abdomen and left leg. Following the injury, he saw his doctor who prescribed cephalexin and doxycycline for treatment of a superficial skin infection at the wire injury site. Unfortunately, the infection progressed, and he developed three subcutaneous (SQ) abscesses along the site of his injury and presented to the hospital for sepsis.
His SQ abdominal and leg abscesses grew Staphylococcus epidermidis and Raoultella planticola but were successfully managed surgically. Although the patient was asymptomatic, and blood cultures remained negative, during workup for his sepsis, an MRI found a 2.3 cm ring enhancing lesion suggestive of an abscess on his frontal lobe. Neurosurgery drained the left frontal abscess, and intraoperative cultures from both his cerebral and intraabdominal abscesses grew the same species of Nocardia farcinica and Staphylococcus epidermidis.
The Infectious disease team empirically prescribed linezolid, trimethoprim-sulfamethoxazole (TMP-SMX), and amoxicillin/clavulanic acid. Most Nocardia spp are sensitive to a combination of these three antibiotics, and the empiric treatment for disseminated nocardiosis includes TMP-SMX with at least one other antibiotic.3 Because this patient had a cerebral abscess, TMP-SMX was chosen due to its excellent central nervous system penetration. Other antibiotics such as carbapenems (imipenem) would be contraindicated in this patient due to their increased seizure risk. Interestingly, the patient had risk factors for developing a frontal abscess such as recurrent sinus infections and numerous dental issues; it is suspected that the Nocardia spread to the cranium hematogenously since it was present in each abscess location.
This case illustrates the importance of determining the causative organism for a given infection. Cerebral nocardiosis represents 2% of all cerebral abscess cases,4 so it may not be the first possibility on the differential. However, a thorough history and critical communication between provider and laboratory are necessary to support antibiotic stewardship and provide patient-centered care.